Streamlined Enrollment Reveals Surprising Efficiency
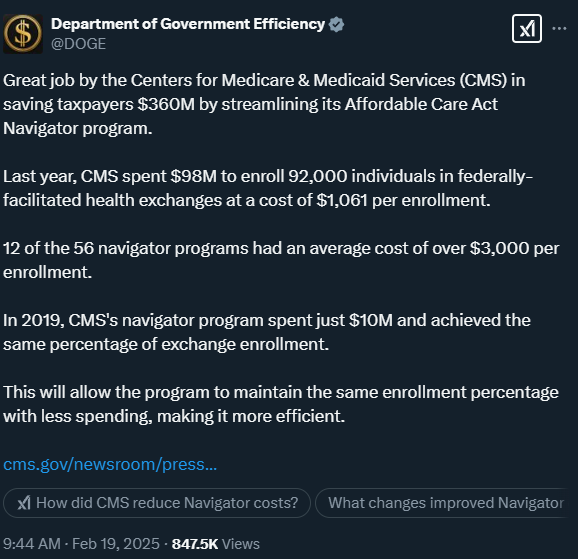
The Department of Government Efficiency (DOGE) has commended the Centers for Medicare & Medicaid Services (CMS) for saving taxpayers $360 million by streamlining its Affordable Care Act (ACA) Navigator program. In previous years, the program spent substantial sums to assist consumers in enrolling in federally facilitated health exchanges, yet the actual number of beneficiaries reached did not always justify the costs. This newly announced cost reduction strategy has prompted fresh discussions on how government agencies can continue providing essential services while minimizing unnecessary spending. By reevaluating operational methods and focusing on data-driven decision-making, CMS has demonstrated that robust enrollment rates can be maintained or exceeded without escalating budgets.
Key Figures and Why They Matter
The numbers behind the streamlined initiative underscore the stark contrast between past and present spending. According to CMS, last year’s outlay reached $98 million to enroll 92,000 individuals, which averaged out to $1,061 per enrollee. Even more noteworthy is the fact that 12 out of 56 navigator programs exceeded $3,000 in cost per enrollee. Critics and policy analysts alike had questioned the sustainability of spending so heavily on outreach services with limited coverage gains.
In sharp comparison, CMS’s 2019 Navigator program achieved the same percentage of overall enrollment for just $10 million. The agency’s recent announcement of $360 million in savings suggests that the adjustments to the program’s structure are not simply superficial changes but rather significant reforms that address possible inefficiencies head-on. This development underscores the importance of continuous audits, transparent reporting, and a willingness to adapt when conventional practices yield diminishing returns.
Potential Outcomes and Far-Reaching Implications
This transformation within the ACA Navigator system could have several broader implications. First, other government departments and programs may see a strong precedent for exploring more data-driven models that reduce costs while maintaining high impact. Second, by demonstrating efficient enrollment processes, CMS also paves the way for future health policy innovations and reforms—encouraging a mindset that significant savings can be attained without compromising on the intended mission of public service.
Moreover, beneficiaries stand to gain from more targeted outreach, as resources can be reallocated toward improving user experience and expanding coverage for underserved communities. Through smarter budgeting and strategic planning, agencies can pinpoint where funds deliver the greatest returns, ensuring that more Americans can access the health care services they need.
How did CMS manage to reduce Navigator costs so drastically?
CMS carefully reviewed how navigators recruited and supported enrollees, identifying areas where in-person outreach and administrative layers could be trimmed without sacrificing enrollment. Automation and increased virtual assistance also contributed to lower operational costs.
What changes improved Navigator efficiency the most?
A shift toward digital platforms allowed navigators to reach more people using fewer resources. By focusing on online enrollment tools and call center expansions instead of costly in-person events, CMS reduced overhead while preserving accessibility for consumers.
Will this new approach affect the quality of enrollment assistance?
If managed properly, the quality of enrollment assistance should remain consistent or even improve. With better tracking and more strategic allocation of funds, navigators can devote time and resources to addressing enrollee needs rather than administrative tasks or inefficient outreach methods.
Does lower spending put underserved communities at risk?
While concerns exist that reducing funding could unintentionally limit outreach in certain areas, CMS has emphasized that the strategy’s primary goal is to align resources where they are needed most. So far, data suggests the same or greater percentage of successful enrollments.
Could other programs learn from CMS’s approach?
Absolutely. The reevaluation and restructuring process undertaken by CMS may serve as a model for other federal, state, and local programs seeking to deliver strong outcomes while optimizing their budgets.
Reflections on Prudent Spending in Public Health
As CMS demonstrates, government programs can meet—or even exceed—their objectives while significantly reducing overhead. DOGE’s spotlight on the $360 million savings signals an ongoing desire to see every federal dollar spent more judiciously. Through targeted outreach, technological upgrades, and transparent financial oversight, agencies can strike a balance between helping the public and keeping spending in check. As this model becomes more commonplace, it’s likely that other sectors will follow suit, bringing greater efficiency and effectiveness to a broad spectrum of government services.